By John N. Galgiani MD | Director, Valley Fever Center for Excellence
Valley Fever (coccidioidomycosis) is one of the three targeted public health problems by the Maricopa County Medical Society’s new Honor Roll Program (read more about this at https://www.mcmsonline.com/announcements/clinician-honor-roll-pledge). With the Honor Roll Program, we hope to recognize those clinicians who master a basic understanding of Valley Fever, seek to diagnose it in their patients, and regularly encourage other clinicians to do the same. That effort received an infusion of new information April 5 of this year as the result of a day-long conference devoted entirely to Valley Fever, the 58th Annual Meeting of the Coccidioidomycosis Study Group, held on the University of Arizona College of Medicine—Phoenix campus. The entire program can be found now and some of the presentations should be available later on the organization’s website, https://coccistudygroup.com. In this article, I have selected a few of the topics that were discussed because they should be of general interest to the Society’s members.
CDC and NIH are committed to study the benefits of early treatment of Valley Fever pneumonia.
At a two-day workshop in Bakersfield CA last September it was announced by the Director of the NIH, Dr. Francis Collins, that the CDC and the NIH were going to conduct a clinical trial of some sort in patients with Valley Fever. At this meeting, Dennis Dixon, Chief of the Bacteriology and Mycology Branch at the National Institute of Allergy and Infectious Diseases, presented the first information about what this study will look like. The question that the NIH study will address is this: does early treatment of uncomplicated coccidioidal pneumonia help patients?
Many patients are surprised to learn that this is actually a completely unsettled issue. Since there was no effective therapy for Valley Fever before the late 1950’s, we know from the clinical course of most patients before then that they will eventually resolve their infections, even though it often takes many weeks to many months and causes considerable loss of time from work or other normal activities. When treatment was the highly toxic and parenterally administered amphotericin B, still only patients with life-threatening or progressive infections elected therapy. However, now we have several orally absorbed and relatively safe azole anti-fungal drugs, such as fluconazole, and so treating patients with less extensive Valley Fever infections is much more feasible. The problem is that there has never been a study to determine how effective early treatment is in either reducing the length of illness or preventing complications. Without such information, opinions vary as to whether all newly diagnosed patients should be treated or whether treatment should be more selectively recommended. The study outlined by Dr. Dixon should address this area of uncertainty.
Most early coccidioidal infections present as community-acquired pneumonia (CAP) and can only be distinguished from bacterial or other etiologies by specific serologic tests or by isolating Coccidioides spp. in culture. This problem of diagnosis is compounded further because serologic tests, although quite specific, may initially be falsely negative and respiratory specimens may not always be available or demonstrate the presence of Coccidioides spp. in culture or by PCR. These details present challenges to designing an early intervention study since treatment is most likely to be effective if started as soon as possible after the onset of symptoms.
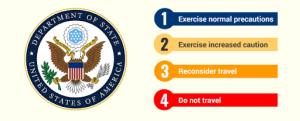
The proposed study will enroll patients in endemic regions for coccidioidomycosis such as Phoenix, when they are first diagnosed with CAP, and before Valley Fever is diagnosed. Subjects who agree to participate will be randomized to receive in a blinded fashion either i) azithromycin plus fluconazole or ii) azithromycin plus a fluconazole placebo. The azithromycin will be continued for two weeks and the fluconazole for 6 weeks, according to the outline in Figure 1. Coccidioidal serology will be obtained at the time of enrollment and two times thereafter and results of these studies will be provided to the investigator and the subject at the end of study.
Although further details are still under development, this synopsis gives a fairly good idea of what direction this announced study will take. One thing is very clear, the support of primary care clinicians in our community will be critical to make such a study successful. Stay tuned as further information becomes available.
A structured approach to patients with protracted fatigue following uncomplicated coccidioidal pneumonia.
As well known by most clinicians who have cared for patients with coccidioidal pneumonia, the symptom of fatigue is often very prominent, even debilitating, and may eventually become the sole complaint as the signs and symptoms of the initial inflammatory process subside. Typically, there is no indication of ongoing tissue destruction and in fact the patient’s general appearance is that of a person in which the problem has resolved. In my experience, patients who have had little or no experience in dealing with a chronic illness are particularly susceptible. They often have high expectations of what they should be doing during the day and the fatigue that they experience is frustrating, occasionally depressing to them. An illustrative example of this situation might be Connor Jackson, the Arizona Diamondback Major League Baseball player who, in May of 2009, was diagnosed with coccidioidal pneumonia. Although public records do not indicate any significant residual damage to his lungs or elsewhere, he was unable to return to the lineup for the rest of the season. Very little is written about how to help patients with this condition, further frustrating patients and clinicians alike.
An approach that has developed at the Valley Fever Center in Phoenix is to address the fatigue as a manifestation of a deconditioned state. The concept here is that because the initial fatigue that is so very common with Valley Fever predictably results in large reductions in usual activities, patients to a greater or lesser extent become deconditioned. Their attempts to conduct activities of daily living, let alone strenuous physical activity, produces fatigue that feels very similar to that which the disease had produced, even after the illness has resolved. There is a practical value of framing the problem in this way. While there is virtually no understanding of the etiology of the disease-induced fatigue, there are many approaches to addressing deconditioning.
A poster presented at the April meeting by the Outpatient Rehabilitation Group at St. Joseph’s Hospital and Medical Center described a developing systematic approach to reconditioning patients with post coccidioidal pneumonia fatigue. As they described, the approach involves multiple modalities, all common to trained physical therapists, that are used in concert and tailored to individual patients, depending upon the specific complaints and goals of each. As described in their presentation, physical therapists provide a structured program and track the improvement that the reconditioning produces over time. This provides concrete documentation to the patient that the condition is improving. Another benefit of referring patients with this condition to a physical therapist is that the therapist creates the treatment plan, relieving the patient of the responsibility for managing his or her own rehabilitation All of these factors contribute to enabling patients to regain control of what otherwise is often perceived of as a hopeless situation.
This program is relatively new; only 20 patients have been enrolled to date. It is planned that with increased experience a structured protocol will emerge which could then be shared with physical therapists across Arizona and elsewhere. Toward that end, the Northern Arizona University Department of Physical Therapy, which has a program in Phoenix, is working with the St. Joseph’s group. It may also be possible and instructive to develop physiologic measurements to better characterize the subjective sensation of fatigue in more objective metrics.
Back to the future: coccidioidal skin testing to be clinically available again this year.
One of the most interesting announcements at the April meeting was made by Stewart Nielsen, President of Nielsen BioSciences, Inc., that his company is going to make a Valley Fever skin testing product, Spherusol®, available for clinical use later this year.
As far back as the 1940’s, it was known that intradermal injection of extracts of Coccidioides spp. produced induration two days later in most patients with a history of past coccidioidomycosis. Commercial coccidioidal skin test material was originally made from extracts of mycelia (coccidioidin) and later in the 1970’s was also produced from spherules (spherulin). However, in the mid 1990’s manufacturers of both products ceased marketing and skin tests for Valley Fever became unavailable.
In recent years, a San Diego-based company, Allermed Laboratories, acquired the previously made stock of spherulin, reformulated it, performed clinical studies demonstrating its safety and efficacy, and has filed it with the FDA as Spherusol®. It has been approved by the FDA for commercial use. The exact date of its availability is not yet certain but likely in the next several months.
How Spherusol® will be used in clinical practice is not yet clear, and Nielsen BioSciences have not yet provided any information on how it intends to educate health care providers. Because a coccidioidal skin test has been unavailable for nearly two decades, most clinicians practicing today have little or no experience using it. There is a technique involved in correctly applying and reading skin tests and this will have to be re-instituted into clinical practice.
Figure 1. NIH preliminary study design.
Back to News